
Letrozole 2,5 mg/tab (UP)
€ 50,00
Op voorraadBuy premium Letrozole (Femara) from Unique Pharma. Lab-tested, fast shipping, competitive prices. Perfect for PCT protocols.
Acne
Yes
Halfwaardetijd
24 Hours
Dosering
12.5-25mg Daily
Detectietijd
12 Days
Aromatisering
N/A
Water Retentie
No
Hepatotoxiciteit
N/A
HBR
N/A
Product Informatie
Over Letrozole 2,5 mg/tab (UP)
1. Description: Clinical summary
Letrozole (active compound: letrozole) is an oral non‑steroidal aromatase inhibitor used primarily in the treatment of estrogen receptor–positive (ER+) breast cancer in postmenopausal women. It reduces circulating and tissue estrogen levels by inhibiting the aromatase enzyme and thereby decreases estrogen-driven tumor growth. Indications include adjuvant therapy for early-stage ER+ breast cancer, treatment of hormone receptor–positive advanced or metastatic breast cancer, and neoadjuvant use to shrink tumors prior to surgery in postmenopausal patients. Letrozole is also used off‑label for ovulation induction in infertility management (short-course use in premenopausal women). It is contraindicated in pregnancy and should not be used during breastfeeding.
2. How does letrozole work?: Mechanism of action
Letrozole is a reversible, non‑steroidal inhibitor of the aromatase enzyme (CYP19A1). Aromatase catalyzes the final step in estrogen biosynthesis, converting androgens (androstenedione and testosterone) into estrogens (estrone and estradiol). By inhibiting aromatase, letrozole markedly lowers peripheral and intratumoral estrogen production in postmenopausal women. Reduced estrogen availability leads to decreased activation of estrogen receptors in ER+ breast cancer cells, thereby slowing tumor growth and promoting tumor regression.
Pharmacokinetics (summary)
- Administration: oral tablets.
- Typical absorption: rapidly absorbed; peak concentrations usually within ~1 hour.
- Half‑life: approximately 2 days (around 40–70 hours in most reports).
- Metabolism: hepatic (primarily CYP3A4 and CYP2A6).
- Excretion: metabolites excreted in urine.
- No routine dose adjustment required for mild–moderate hepatic or renal impairment, but use caution in severe impairment and consult product labeling.
3. Dosage: Medical and varying usage guidelines
Always individualize dosing to the patient and follow local prescribing information or specialist guidance.
Oncologic (approved) uses in postmenopausal women
- Standard adult dose: 2.5 mg orally once daily.
- Adjuvant therapy (early-stage ER+ breast cancer): typically 2.5 mg daily for 5 years. In some situations, extended therapy (up to 10 years or switching strategies) is considered based on guideline recommendations and individual risk.
- Metastatic (advanced) disease: 2.5 mg daily until disease progression or unacceptable toxicity.
- Neoadjuvant therapy (tumor downstaging prior to surgery): 2.5 mg daily for several months (often 3–6 months), depending on response and surgical planning.
Off‑label fertility use (ovulation induction in premenopausal women)
- Typical regimen: 2.5 mg once daily for 5 days (commonly cycle days 3–7 or 5–9); some protocols use 5–7.5 mg/day for 5 days in patients who do not respond to lower doses. Use only under specialist reproductive medicine supervision. Confirm non‑pregnancy before use and avoid conception during treatment unless used specifically for ovulation under controlled conditions.
Special populations and dose adjustments
- Renal impairment: no routine adjustment for mild–moderate impairment; limited data in severe impairment—use caution.
- Hepatic impairment: no adjustment typically required for mild–moderate hepatic impairment; use caution in severe hepatic dysfunction and consult product information.
- Elderly: no routine adjustment solely for age.
- Pediatric: not generally indicated.
- Missed dose: take as soon as remembered on the same day; do not double the next dose.
Concomitant therapy considerations
- Avoid concurrent estrogen or estrogen-containing products, which may antagonize therapeutic effect.
- Evaluate drug–drug interactions (see section on interactions). Use caution with strong CYP3A4 inducers or inhibitors.
4. Side effects: Common and rare bad effects
Common (frequency varies; seen in clinical trials and practice)
- Hot flashes and sweats
- Musculoskeletal pain: arthralgia, myalgia, stiffness
- Bone mineral density loss, increased risk of osteopenia/osteoporosis and fractures (important long‑term risk)
- Fatigue, weakness
- Nausea, vomiting, decreased appetite
- Headache
- Vaginal dryness, dyspareunia, decreased libido
- Increased serum cholesterol or unfavorable lipid changes
- Insomnia, mood changes (depression, irritability)
Less common / uncommon
- Skin reactions (rash, pruritus)
- Hair thinning (alopecia)
- Peripheral edema
Rare but serious (require prompt medical attention)
- Significant bone fracture due to osteoporosis (monitor BMD)
- Severe hypersensitivity or anaphylaxis (very rare)
- Hepatic dysfunction or clinically significant transaminase elevations (rare)
- Severe skin reactions (exceedingly rare)
- Ischemic cardiovascular events have been reported—evaluate baseline cardiovascular risk and monitor as clinically indicated
Monitoring-related adverse considerations
- Long‑term estrogen suppression increases risk of bone loss; consider baseline and periodic bone mineral density (DEXA) assessment and bone‑protective measures when indicated.
- Monitor lipids and manage dyslipidemia per guidelines.
Patient counseling highlights
- Advise women of childbearing potential to avoid pregnancy and use effective contraception while taking letrozole and for a recommended period after discontinuation (follow local obstetric guidance). Letrozole is teratogenic.
- Report new or worsening bone pain, acute limb pain/swelling (possible DVT), severe shortness of breath, jaundice, or rash promptly.
5. Storage: HOW to store it
- Store letrozole tablets at controlled room temperature (typically 20–25°C / 68–77°F) unless the product label specifies a slightly broader range (e.g., 15–30°C).
- Protect from excessive heat, moisture, and light. Keep in original container with child‑resistant cap if provided.
- Keep out of reach of children and pets.
- Do not use past the expiration date printed on the package.
- Dispose of unused tablets or expired medication safely according to local regulations (do not flush; use community take‑back programs if available).
Important safety reminders (concise)
- Contraindicated in pregnancy and breastfeeding; avoid in pregnant women and ensure negative pregnancy test before initiating in premenopausal use for fertility.
- Primarily indicated for postmenopausal women with hormone receptor–positive breast cancer. Off‑label fertility use requires specialist oversight.
- Monitor bone health and cardiovascular risk factors during therapy; consider calcium + vitamin D and bone‑targeted therapy (bisphosphonates or denosumab) when indicated by bone density results and risk assessment.
- Review concomitant medications for potential CYP3A4/CYP2A6 interactions and avoid concurrent estrogen therapy.
For prescribing decisions, monitoring intervals, or management of adverse effects tailored to an individual patient, consult relevant clinical guidelines (oncology and reproductive medicine) and the official product labeling.
Dosering
Aanbevolen
12.5-25mg Daily
Halfwaardetijd
24 Hours
Voordelen
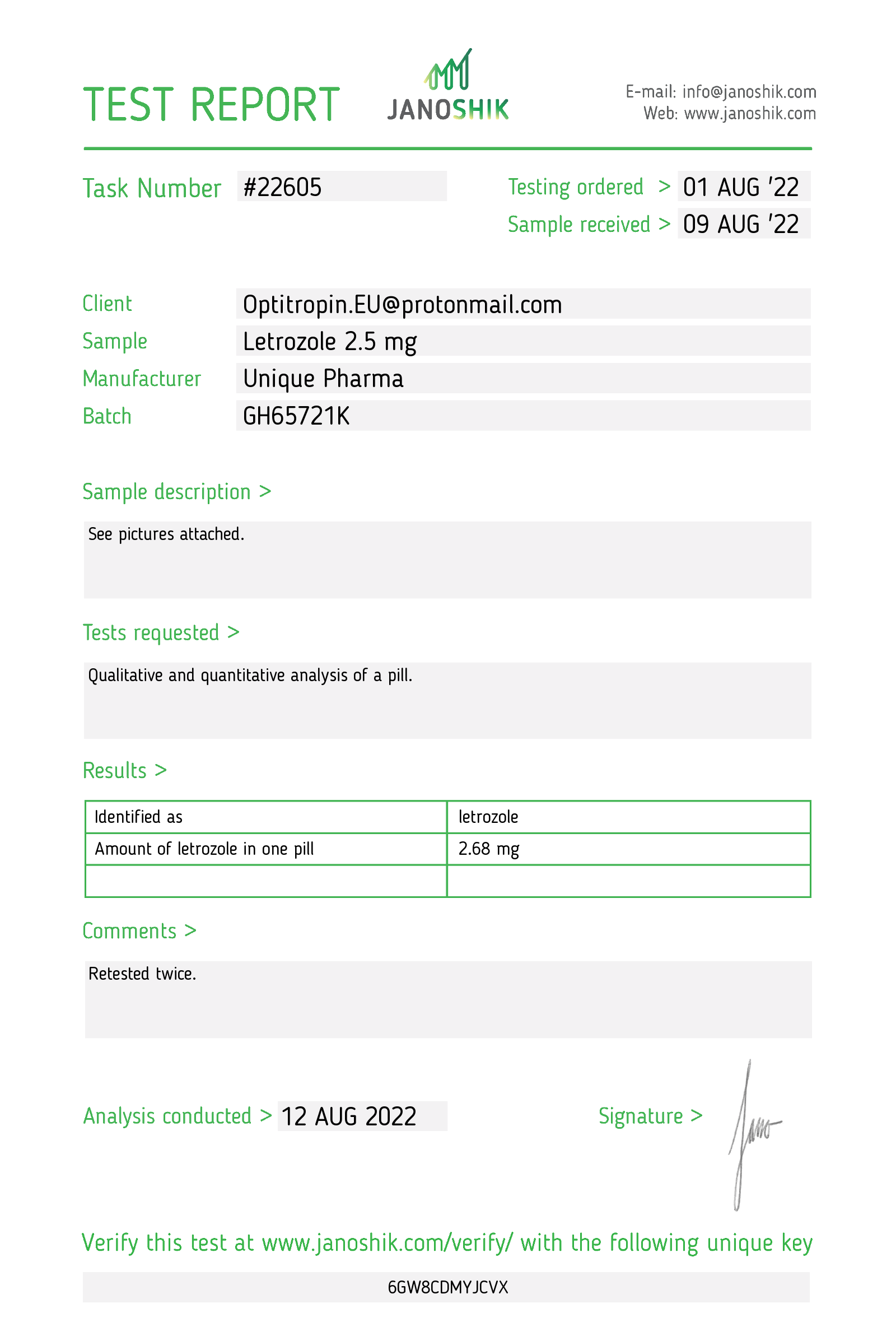
- Laboratorium getest op zuiverheid
- Farmaceutische kwaliteit gegarandeerd
- Discrete en veilige verzending
- Uitstekende klantenservice
- Snelle levering in heel Europa
Gratis verzending
Gratis verzending bij bestellingen boven de €200.
Leveringsgarantie
Gratis herverzending als uw bestelling niet aankomt.
Snelle levering
Verzending binnen 24u. Levering 48-72u in NL & BE.
Bitcoin Betaling
Betaal veilig en blijf volledig anoniem met Bitcoin.
Veilig afrekenen
Beveiligde SSL-verbinding voor alle transacties.
Authentiek
Originaliteitscontrole voor al onze producten.